Repetitive deep TMS in alcohol dependent patients halts progression of white matter changes in early abstinence.
Stopping the white matter damage can reduce relapse in Alcohol Use Disorder patients.
• Chronic alcohol consumption produces alterations in brain microstructure that are notable in the white matter and progress even during abstinence.
• Researchers at the Institute for Neurosciences manage to protect patients’ white matter using Transcranial Magnetic Stimulation (TMS).
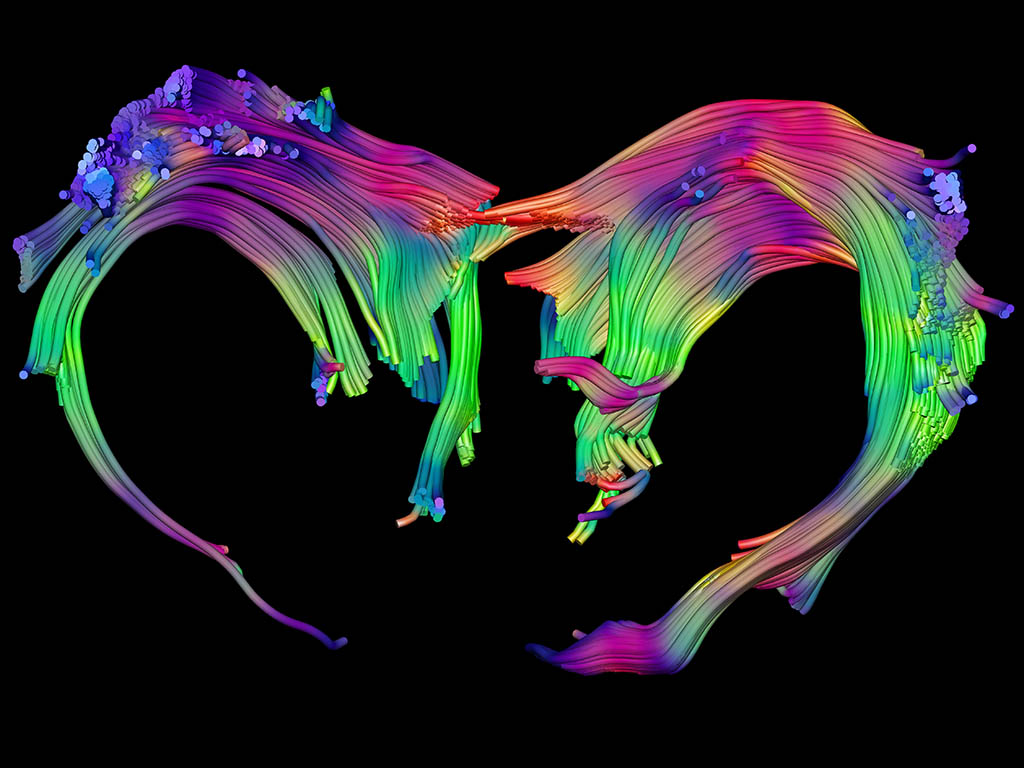
(Photo: Santiago Canals, Mohamed Selim, and Silvia De Santis, IN-CSIC-UMH researchers)
Watch video on our YouTube channel: attached icon ‘Link to YouTube’
A study led by the Institute for Neurosciences (IN), a joint center of the Spanish National Research Council (CSIC) and the Miguel Hernández University (UMH) of Elche, has found a way to stop the progression of white matter deterioration of the brain of patients with Alcohol Use Disorder, which is associated with a decrease in relapse. This work, published in the journal Psychiatry and Clinical Neurosciences, demonstrates that the alteration of white matter is a central characteristic of the pathology, and not a collateral damage of alcohol consumption, and opens a new therapeutic avenue to prevent relapse.
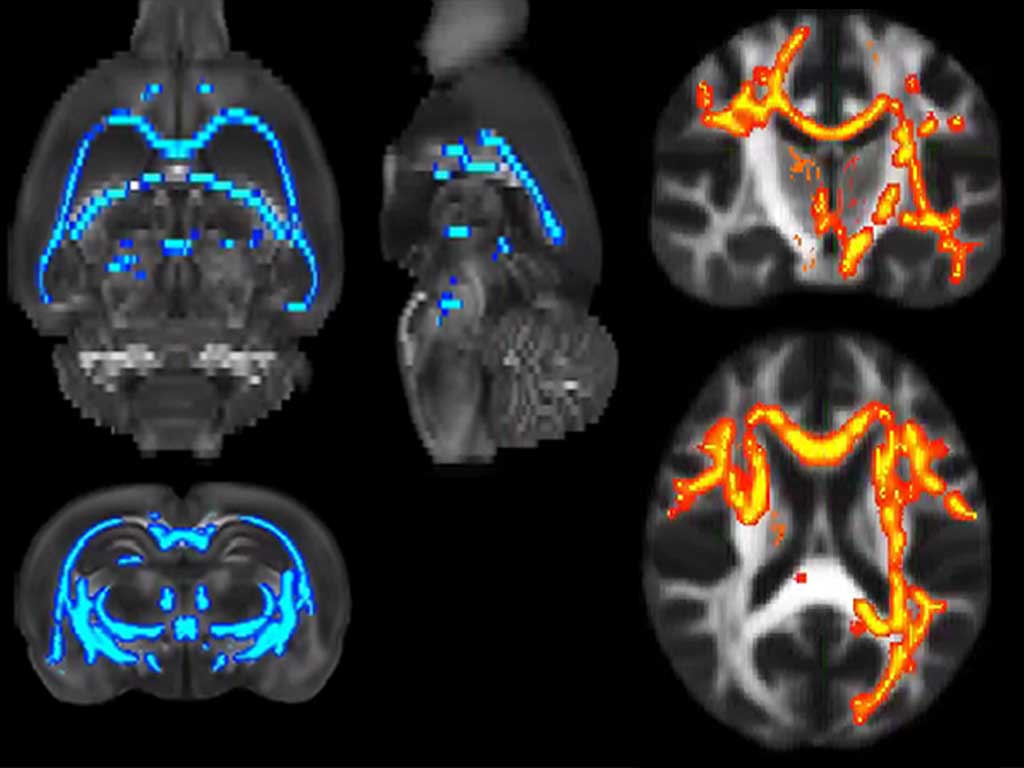
Researchers from Plasticity of Brain Networks and Translational Imaging Biomarkers laboratories at the IN, led by Santiago Canals and Silvia De Santis respectively, already demonstrated a few years ago that alcohol consumption causes damage to the white matter of the brain and that this damage does not stop when patients stop drinking, but rather progresses very strikingly during abstinence. In this work, they have not only reproduced the data from that previous research in a new group of patients, but they have applied a non-invasive method based on Deep Transcranial Magnetic Stimulation (Deep TMS) that prevents the progression of white matter damage during abstinence.
“It is a non-invasive neuromodulatory technique that consists of applying a magnetic field repeatedly to the head. Thus, an electric field is generated that increases excitability and activates large populations of neurons”, explains Mohamed Selim, the first author of the article. Furthermore, the researcher highlights that TMS, despite not being a simple technique to perform from a clinical point of view because it requires specific facilities, has previously been used to treat other addictions, such as smoking, and has generated positive results.
Longitudinal study in patients
In this study, in which researchers from Ben-Gurion University (Beer Sheva, Israel), the Linköping University Hospital (Sweden) and the Central Institute of Mental Health (Mannheim, Germany) also participated, experts have applied the TMS treatment periodically for several weeks to a group of patients, made up of men and women who were in the process of detoxification. Furthermore, to rule out a possible placebo effect, a simulation of this stimulation was performed on a group of control patients.
The researchers recorded images of the brain before starting the intervention and after receiving the treatment. Indeed, they confirmed that only in those patients who had received stimulation, TMS had been enough to stop the progression of the alteration in the microstructure of the white matter that occurs when patients stop drinking. And, even more significantly, their relapse rates decreased three months after treatment, so these are stable long-term results.
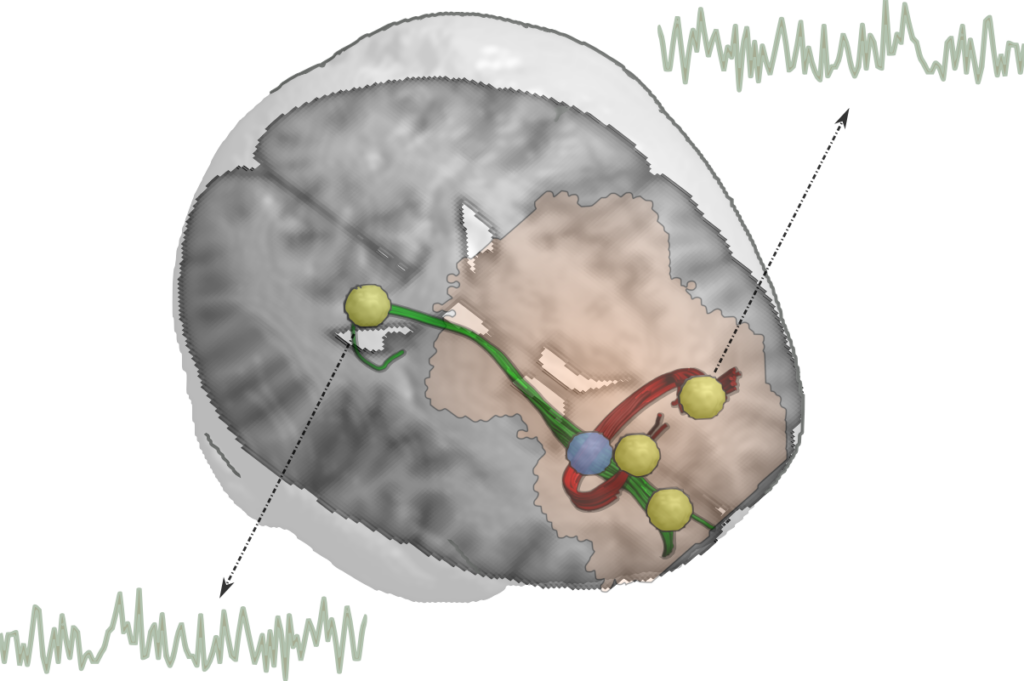
A brain reconstructed from patient data in which the region where TMS most significantly protects white matter has been highlighted in blue. The pale pink hat marks the area of influence of the TMS. The blue region contains the nerve fibers (green and red) that connect several brain areas (yellow) whose activity is normally altered in patients and that the TMS intervention normalizes. IN-CSIC-UMH.
The results obtained are the result of an international collaboration that has allowed several research groups to share their expertise on Alcohol Use Disorder. IN researcher Santiago Canals highlights the importance of collaboration between experts: “Thanks to the fact that we are a large consortium, we have been able to combine TMS technology, structural and functional brain imaging, and clinical experience and perspective along with basic experimentation. Without all these legs, a translational research structure is not sustained when it aims to have a real impact in the clinic.”
The White Matter
Alcohol use disorder is the most prevalent form of addiction, characterized by excessive and prolonged alcohol consumption. This addiction has a great burden on society, since, among the population aged 15 to 49, 3.8% of female deaths and 12.2% of male deaths are attributed to alcohol consumption worldwide. It is a chronic illness that alternates cycles of sobriety and relapse. Therefore, the main challenge, along with prevention, is to break these cycles to prevent consumption again.
White matter, the tissue that connects the different brain regions, is made up of axons that connect neurons and glia cells that accompany them, performing several functions. “One of these functions is the production of myelin that wraps the axons and ensures their correct functioning,” says IN researcher Silvia De Santis, and adds: “The alteration of the microstructure that we found in the patients correlated with the level of alcohol consumption. “In addition, we found the same result in two different animal models in which we had previously investigated, which allowed us to study the biological bases of this change, and discover that they were associated with a decrease in myelin”.
The evidence accumulated by the team pointed to the white matter as a possible therapeutic target: “Our reasoning was that brain stimulation, by a process known as myelin plasticity, could regenerate the white matter of patients and thereby protect the brain and prevent patients from relapse,” highlights Mohamed Selim. When the cells that produce myelin detect neuronal activity, they react by producing more myelin. In addition, progenitor cells mature, so there are more cells with the capacity to myelinate axons.
After verifying that, when applying the TMS treatment, the areas of the stimulated white matter were protected during abstinence, the researchers verified that they also recovered their function. The communication between protected brain regions was more similar to the healthy subjects than in subjects with alcohol use disorder. The patients reported less craving for consumption and it was possible to record, after 3 months, that the relapse had decreased.
Now researchers plan to study the mechanism of plasticity in detail in order to propose even more effective therapies. “Our goal now is to refine brain stimulation protocols and combine them, possibly with pharmacological treatments, aimed at maximizing the therapeutic window that we have discovered,” explains Canals.
This work has been possible thanks to funding from the Horizon 2020 Research and Innovation Program of the European Union, the Ministry of Science and Innovation of Spain, the Spanish National Research Agency, the Severo Ochoa R&D Centers of Excellence Program, the Generalitat Valenciana, through the PROMETEO and CIDEGENT scholarships, the Swedish Research Council, ”la Caixa” Foundation and the Marie Skłodowska-Curie-COFUND agreement.
Source: Institute for Neurosciences CSIC-UMH (in.comunicacion@umh.es)

 Español
Español