Whole transcriptome analysis of peripheral blood mononuclear cells from de novo and drug-naïve Parkinson’s disease patients.
Researchers at the IN UMH-CSIC move closer to an early diagnosis of Parkinson’s disease through a simple blood test
• Using sequencing and bioinformatic analysis, scientists identified 22 genes with altered expression in drug-naïve Parkinson’s patients, many of which are linked to immune and iron-related pathways.
• The study, published in Neurotherapeutics, paves the way for blood-based diagnostic tools to detect Parkinson’s disease at earlier stages.
(Photo: UMH Professor Jorge Manzanares, who leads the Translational Neuropsychopharmacology of Neurological and Psychiatric Diseases Group at the Institute for Neurosciences).
The genetic analysis of a blood sample could become a tool for the early diagnosis of Parkinson’s disease, according to an exploratory study led by researchers from the Institute for Neurosciences (IN), a joint center of the University Miguel Hernández (UMH) of Elche and the Spanish National Research Council (CSIC). Although not yet available for clinical use, the method was tested in newly diagnosed patients and proved effective, offering a non-invasive way to detect and monitor disease progression before major symptoms appear.
The results, published in the journal Neurotherapeutics, stem from the collaboration between scientists from the Translational Neuropsychopharmacology of Neurological and Psychiatric Diseases Group, led by UMH Professor Jorge Manzanares and the Cellular Plasticity and Neuropathology Laboratory, both at the IN; the Institute for Health and Biomedical Research of Alicante (ISABIAL), the Carlos III Health Institute, and Madrid’s Hospital 12 de Octubre.
Parkinson’s disease affects around 12 million people worldwide. It is the second most common neurodegenerative disorder and one of the leading causes of neurological disability. One of the most significant challenges in Parkinson’s research is achieving a diagnosis before severe motor symptoms emerge.
Currently, diagnosis begins with a clinical examination when visible symptoms appear. “However, tremors occur when neurological damage is already advanced and may be mistaken for other disorders”, explains Manzanares. “Until recently, the only definitive diagnosis came from post-mortem tissue analysis, but it is crucial to develop fast, minimally invasive methods that detect the disease earlier”.
The method developed by the researchers requires only a blood draw. The analysis, performed with equipment already available in many hospital laboratories, identifies genetic alterations associated with the disease in its earliest stages.
“The key lies in genetically analyzing a type of immune cells called peripheral blood mononuclear cells”, explains Professor Francisco Navarrete, first author of the article. Like all cells, these contain genetic information, but not all genes are active at all times. Some genes switch on or off depending on the body’s needs, such as during an infection or the development of a disease.
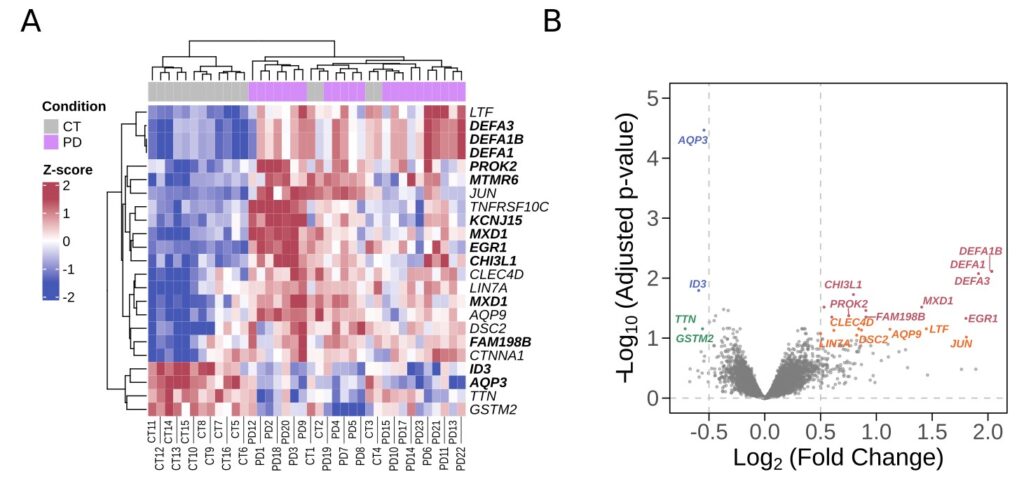
Changes in gene expression in Parkinson’s disease. A) In red, increased gene expression; in blue, decreased expression. Genes with the most significant changes are shown in bold. B) Most significant upregulated genes in red, followed by pink, blue, and green, respectively. Source: Neurotherapeutics.
Through sequencing and bioinformatics, the researchers identified more than 20 genes whose activity was altered in untreated patients with Parkinson’s disease. “These changes are not seen in healthy individuals”, notes Marina Guillot, predoctoral researcher who led the gene expression analyses together with CSIC scientist José P. López-Atalaya. “This suggests that they could serve as reliable markers for diagnosis and also provide clues about the biological mechanisms underlying disease development and progression”, he adds.
In total, 22 genes showed differential expression between Parkinson’s patients and healthy volunteers. Some are involved in immune responses, supporting the hypothesis that inflammation and the immune system play a role in the disease’s development. Others are linked to molecular transport within brain tissue and iron homeostasis, processes previously associated with neurotoxicity.
Beyond gene expression, the researchers detected changes in cellular pathways associated with survival, inflammation, cell death, and the composition of immune cells. “We still do not fully understand how Parkinson’s disease emerges and progresses, and current treatments have limited effects”, says Manzanares, who hopes these analyses will help design more effective, personalized therapies in the future.
The exploratory study included 23 patients with Parkinsonism and 16 healthy controls. Despite the small sample size, the findings are consistent with other independent studies conducted in Italy and the United States over the past decade, confirming the diagnostic potential of this approach.
The project was supported by ICAR Foundation, ISABIAL, the Ministry of Education, Vocational Training and Sports, the Tatiana Pérez de Guzmán el Bueno Foundation, the Spanish State Research Agency, the Generalitat Valenciana (Prometeo Program), and the Spanish Ministry of Science, Innovation and Universities.
Source: UMH Communications Service / Institute for Neurosciences UMH-CSIC (in.comunicacion@umh.es)

 Español
Español