Cannabidiol modulates brain molecular alterations, gut microbiota dysbiosis and alcohol self-administration in a mouse model of fetal alcohol spectrum disorder.
Study by the Institute for Neurosciences UMH–CSIC shows that CBD reverses damage caused by fetal alcohol spectrum disorder in mice
• The study, published in Biomedicine & Pharmacotherapy, shows that CBD reverses alterations in the gut–brain axis and gut microbiota caused by prenatal alcohol exposure.
• Cannabidiol treatment normalises anxiety, depression, and increased vulnerability to addiction in mice exposed to alcohol during development, with particularly strong effects in females.
Photo: From top to bottom: Jorge Manzanares (IN UMH-CSIC), Mª Carmen Collado (IATA-CSIC), Raúl Cabrera-Rubio (IATA-CSIC), and Francisco Navarrete (IN UMH-CSIC).
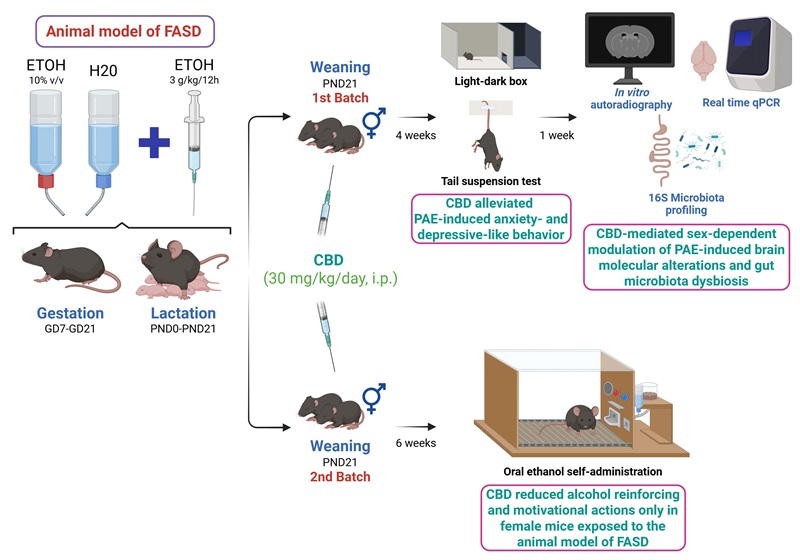
Cannabidiol (CBD) could become a therapeutic tool to treat some of the most common and disabling effects of fetal alcohol spectrum disorder (FASD) caused by alcohol exposure during pregnancy. This is one of the main conclusions of a study conducted in mice and led by researchers from the Institute for Neurosciences (IN), a joint research centre of Miguel Hernández University of Elche (UMH) and the Spanish National Research Council (CSIC). The study also involved researchers from the Institute of Agrochemistry and Food Technology (IATA-CSIC) and the University of Turku (Finland).
The research, published in the journal Biomedicine & Pharmacotherapy, shows that CBD treatment normalises emotional behaviour and vulnerability to addiction in animals exposed to alcohol during the perinatal period, with particularly marked effects in females. Additionally, the treatment significantly improves alterations in gut microbiota composition, promoting a more balanced profile associated with improved intestinal health.
Fetal alcohol spectrum disorder is the leading preventable cause of intellectual disability worldwide and occurs when the developing brain is exposed to alcohol at any point during pregnancy. Its consequences include learning difficulties, emotional disturbances, increased risk of anxiety and depression, impaired behavioural regulation, and, in adulthood, a higher vulnerability to addictive behaviours.
“Despite its enormous social and public health impact, there is currently no approved pharmacological treatment that targets the root cause of the disorder. Available interventions only help manage some symptoms”, explains Jorge Manzanares, principal investigator of the study and head of the Translational Neuropsychopharmacology of Neurological and Psychiatric Diseases laboratory at the IN UMH-CSIC. For this reason, the multidisciplinary research team explored therapeutic strategies capable of correcting alcohol-induced alterations during development.
The relevance of the endocannabinoid system
The study focuses on the endocannabinoid system, a network of molecules and receptors in the nervous system involved in regulating essential processes such as emotion, motivation, learning, and stress responses. Previous independent research has shown that this system is profoundly disrupted following prenatal alcohol exposure, contributing to emotional disturbances and increased addiction risk.
“Cannabidiol, or CBD, a non-addictive compound derived from the cannabis plant, modulates this system and has demonstrated neuroprotective, anti-inflammatory, and anxiolytic properties in other models of neurological damage”, notes the UMH professor. “We therefore set out to first determine the emotional effects of perinatal alcohol exposure in mouse models, identify biomarkers to quantify alcohol’s impact on the brain, and analyse how gut microbiota composition is affected, before testing a chronic CBD treatment administered from weaning and assessing its effects”.
“We found that fetal alcohol spectrum disorder causes not only direct brain damage, but also a systemic disruption affecting intestinal health, and that CBD can modulate this complex cascade of alterations”, Manzanares adds. In the experimental model, mice of both sexes exposed to alcohol during the perinatal period developed behaviours equivalent to anxiety and depression. In females only, this exposure also led to increased motivation to consume alcohol.
Early and continuous CBD administration normalised emotional effects in both sexes. In females, CBD also eliminated vulnerability to alcohol addiction: their motivation to drink was reduced to levels comparable to control animals that had not been exposed to alcohol. The treatment also modulated key brain biomarkers, including dopaminergic and endocannabinoid receptors, whose disruption is associated with emotional and addictive disorders.
CBD treatment normalises emotional behaviour and vulnerability to addiction in animals exposed to alcohol during the perinatal period, with particularly strong effects in females. Source: Biomedicine & Pharmacotherapy.
The gut–brain axis
Another major novelty of the study is its focus on the gut–brain axis. “In both health and disease, there is constant bidirectional communication between the digestive and nervous systems that influences physical and mental health”, explains Francisco Navarrete, first author of the article. This communication occurs through neural, hormonal, and immune signals and is strongly influenced by the gut microbiota. “What happens in the gut microbiota affects the brain, and vice versa”, he adds.
The team found that alcohol exposure during development induces gut dysbiosis —an imbalance in microbial composition— which CBD was able to reverse. Treatment restored microbial diversity and increased the abundance of bacterial populations associated with improved gut–brain communication.
However, these effects differed between males and females, as they naturally exhibit distinct microbial profiles. In this regard, Raúl Cabrera-Rubio (IATA-CSIC) explains that “gut microbiota in mice was influenced by alcohol exposure and modulated by CBD treatment in a sex-dependent manner, and these changes were associated with markers linked to both brain function and other body systems.”
Along similar lines, Navarrete highlights that the findings suggest that some of the sex differences in vulnerability to fetal alcohol spectrum disorder may originate in the gut rather than the brain. The team also identified sex-dependent differences in the expression of genes related to the endocannabinoid system. “These results indicate that gut microbiota actively contributes to the effects of fetal alcohol spectrum disorder and that restoring it could help correct some of its impact on the nervous system as a whole”, he adds.
Mª Carmen Collado (IATA-CSIC) emphasises that although the results are based on an animal model, “our data show that sex modulates both microbiota composition and responses to interventions”. She notes that these findings “reinforce the importance of considering sex as a key biological variable when developing microbiota-targeted strategies, both pharmacological and dietary, as a step toward personalised medicine and nutrition”.
The researchers stress that these findings come from a preclinical animal model and “should under no circumstances be interpreted as a recommendation to self-medicate with CBD, nor as a way to counteract the effects of alcohol during pregnancy”, Navarrete warns. Fetal alcohol spectrum disorder can only be prevented by completely avoiding alcohol consumption during pregnancy.
This research was funded by the Carlos III Health Institute, the Alicante Health and Biomedical Research Institute (ISABIAL), and the Primary Care Addiction Research Network (RIAPAd) of the Spanish Ministry of Health, as well as by the Ministry of Science, Innovation and Universities (MAMI Plus project), the Severo Ochoa Centres of Excellence and María de Maeztu Units programme of the Spanish State Research Agency, and the Valencian Regional Government through the GenT Plan (CDEIGENT 2020–02).
Source: UMH Communication Office (comunicacion@umh.es) / Institute for Neurosciences UMH-CSIC (in.comunicacion@umh.es)


 Español
Español